Possible causes for irritable bowel syndrome
06/27/2018 Food Intolerances

Irritable bowel syndrome (IBS) is a chronic disease of the intestine that causes recurrent abdominal pain and discomfort. In the Western world 10–20 % of the population are affected. For a long time, the diagnosis was mostly based on the exclusion of other severe intestinal diseases. In order to distinguish between different subtypes of IBS several criteria have been established: There are clinical pictures with predominant diarrhea, with constipation and mixed types with alternating episodes of diarrhea and constipation (see figure 1).
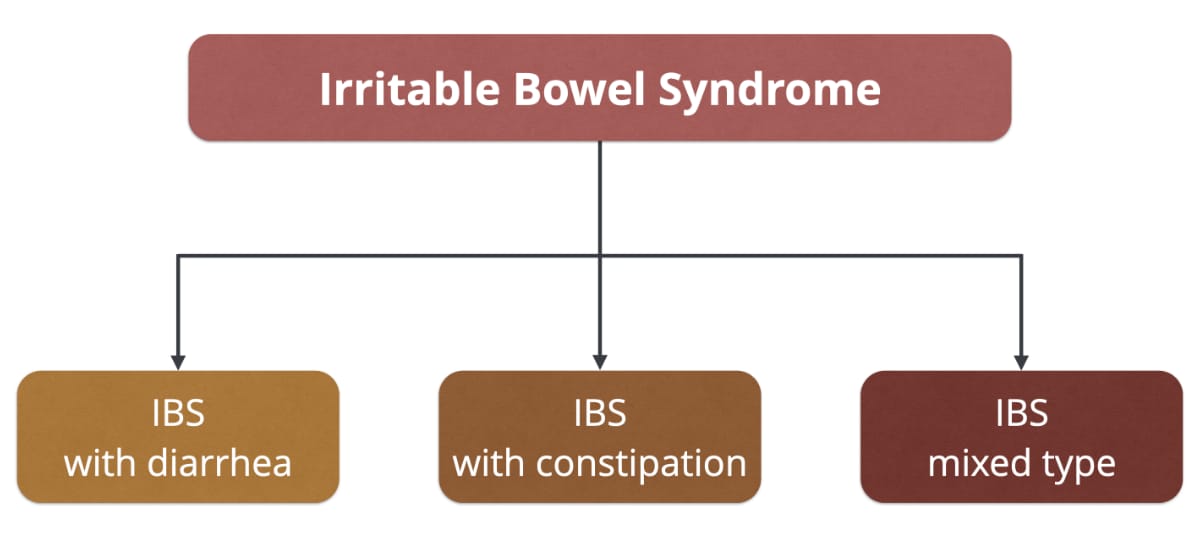
▲ Figure 1: Classification of different IBS subtypes.
Possible causes of IBS
To date, the exact causes of IBS are still unclear, but it is very likely that IBS is caused by a combination of different disorders. Usually, there are no visible signs of intestinal inflammation or tissue damage. Therefore, IBS has been long considered as a pure psychological disorder. But in the last years this point of view started to change – psychological factors, as well as organic factors are involved. In the following, we give an overview over the possible causes of IBS:
Intestinal dysbiosis
Our digestive tract is colonized by an incredible number of microorganisms that form a beneficial symbiosis with us. The administration of antibiotics, infections, preservatives, environmental pollutants, lack of contact with environmental germs and an unhealthy diet can seriously disrupt the composition of the intestinal microbiome. Adverse changes of the microbiome may play a crucial part in the development of IBS, one example being the bacterial overgrowth of the small intestine (SIBO). This can lead to the fermentation of certain carbohydrates in the small intestine, which is not designed to cope with it. Serious side-effects, e.g. bloating and diarrhea, are the consequence. The microbiome is also important for the integrity of the intestinal barrier, which prevents the intrusion of undesirable substances.
Increased visceral sensitivity
IBS patients often experience an increased sensitivity to intestinal stretch stimuli. In general, the small intestine reacts more sensitive to stretching than the large intestine. SIBO can lead to a significant production of gas in the small intestine due to the bacterial fermentation of undigested carbohydrates. This can be a cause of severe abdominal discomfort. The large intestine can be stretched by intestinal gases as well as by the abnormally increased volume of watery stools. Typically, defecation provides relief from the symptoms.
Abnormal motility of the gut
The chyme is slowly passed through the small intestine by muscle contractions. Depending on its composition, the nutrition travels through it at different velocities. Irritable bowel syndrome is often accompanied by an impaired gut motility, causing the chyme to be transported either too slowly or too fast. Reduced gut motility causes a visibly bloated belly, because the intestinal gas isn't removed properly. Despite the reduced motility, the stool may not be drained properly and both constipation as well as diarrhea can occur. An abnormally increased motility reduces the exposure time of the digestive enzymes. Incompletely digested fats and gallic acid that couldn't be reabsorbed properly may then be the cause of fatty stools and diarrhea.
Low-grad inflammation of the intestinal wall
Post infectious IBS may develop as a secondary effect of infections with certain pathogenic germs. Affected individuals frequently suffer from depressions and other psychological disorders. The symptoms are presumably induced by an ongoing low-grade intestinal inflammation.
Increased number of mast cells in the intestinal wall
New research indicates that up to 25 % of IBS sufferers have an abnormally increased number of mast cells and other immunological cells in the intestinal mucosa. These cells are often situated next to sensitive nerve endings, which may explain some of the severe consequences that are caused by the activation of these cells.
Gut-brain axis
The connection between the gut and the brain is an important aspect in the development of IBS. Studies showed that the gut can influence the signal processing in the brain – and this connection also works in the reverse direction. Emotional stress can trigger the release of inflammatory mediators that increase the permeability of the intestinal wall. This can set off a real cascade of adverse reactions if foreign substances enter the blood stream.
IBS patients suffer disproportionally often from depression. Studies showed that the predominant proportion develops gastrointestinal symptoms prior to the affective disease. Nevertheless, the reverse order is also possible and IBS can be the result of a personal tragedy or trauma.
Role of histamine, FODMAPs and other dietary factors
Many IBS sufferers associate their symptoms with certain foods. However, the role of the diet was unclear for a long time. Only recently new studies from a group of Australian scientists revived the discussion: they found out that certain poorly absorbable short-chain carbohydrates and sugar alcohols (so called FODMAPs) trigger symptoms in many IBS sufferers. In fact, many patients suffer from lactose intolerance or fructose malabsorption, but the complaints can occur irrespective of these diagnoses. The low FODMAP diet is an approach that goes further than the avoidance of fructose and lactose and is propably the most promising dietary approach to reduce symptoms of irritable bowel syndrome.
But there are also other dietary factors that have to be considered. The following illustration gives an overview of potential dietary triggers for IBS symptoms.
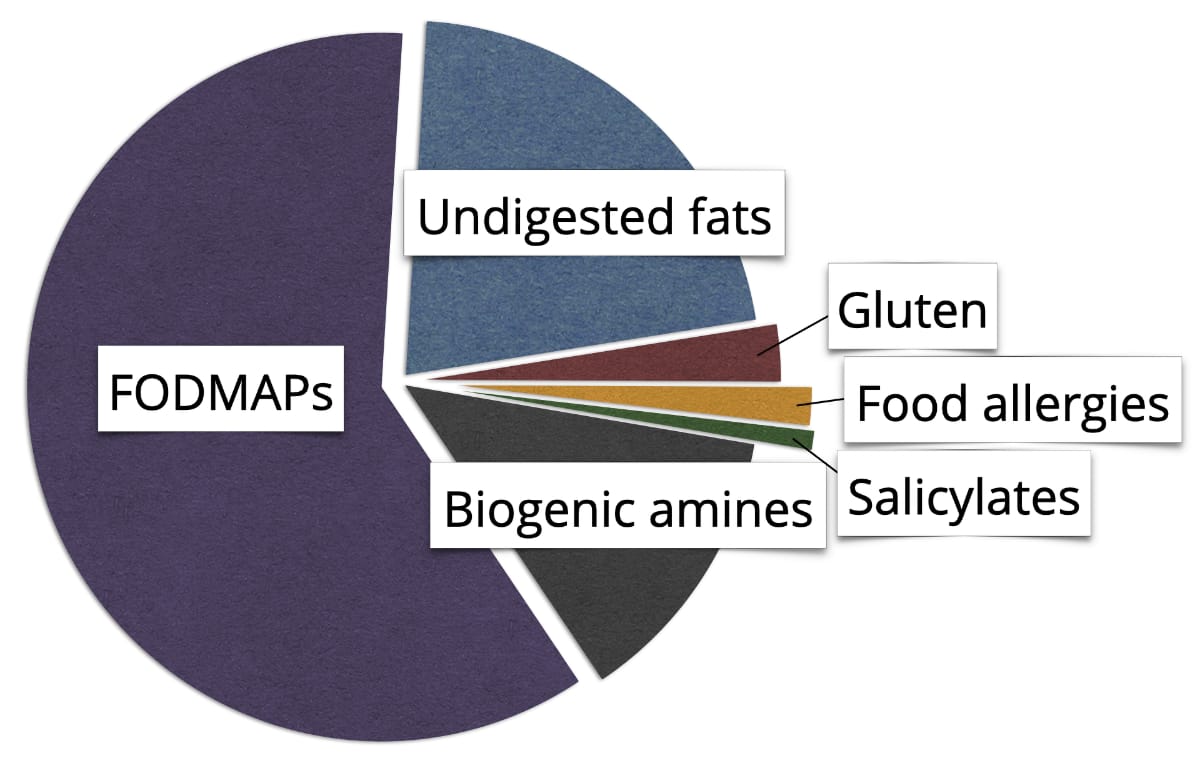
▲ Figure 2: Possible dietary triggers of IBS.
Up to 25 % of IBS sufferers may be sensitive to histamine and other biogenic amines. Real food allergies on the other hand are rare, only 2 % of the IBS sufferers are affected. It remains unclear if and to what extent salicylates play a role.
As IBS is such a wide-ranging disease pattern with different causes, dietary strategies to manage it vary a lot and have to be adopted individually. Diarrhea can be caused by undigested fats and gallic acids, therefore, it is helpful to eat small portions and avoid fatty meals or fried foods. Alcohol is very poorly tolerated by people with diarrhea predominant IBS and should be widely avoided.
 Our price-winning "Food Intolerances" app helps you manage your diet. Available for iOS and Android. Check it out:
Our price-winning "Food Intolerances" app helps you manage your diet. Available for iOS and Android. Check it out:Share article
Back to blog
References:
A. Ford et al., Irritable Bowel Syndrome, N Engl J Med 376 (2017), 2566–2578
M. van Tilburg et al., Which psychological factors exacerbate irritable bowel syndrome? Development of a comprehensive model, Journal of Psychosomatic Research 74 (2013), 486–492
N. Principi et al., Gut dysbiosis and irritable bowel syndrome: The potential role of probiotics, Journal of Infection 76 (2018), 111–120
D. Schumann et al., Low fermentable, oligo-, di-, mono-saccharides and polyol diet in the treatment of irritable bowel syndrome: A systematic review and meta-analysis, Nutrition 45 (2018), 24–31
O. Leiß, Fiber, Food Intolerances, FODMAPs, Gluten und funktionelle Darmerkrankungen – Update 2014, Z Gastroenterol 52 (2014), 1277–1298
Image:
Photo by Olivier Collet on Unsplash
![[Blog]](../../rw_common/images/baliza_logo_retina.png)

