Probiotics and food intolerances: some interesting facts
Our intestinal tract contains around 39 trillion microorganisms that help us break down indigestible food components – fiber, for example – for the body to make use of them. Most of the intestinal flora is found in the large intestine. Over time, the metabolic processes of many lactic acid bacteria and bifidobacteria have become closely interlinked with our own, resulting in a symbiosis that benefits both the bacteria and the host. The bacteria get nutrients and a fertile place to multiply and in return form vitamins and short-chain fatty acids that are essential for many bodily functions.

Our intestinal tract contains around 39 trillion microorganisms that help us break down indigestible food components – fiber, for example – for the body to make use of them. Most of the intestinal flora is found in the large intestine. Over time, the metabolic processes of many lactic acid bacteria and bifidobacteria have become closely interlinked with our own, resulting in a symbiosis that benefits both the bacteria and the host. The bacteria get nutrients and a fertile place to multiply and in return form vitamins and short-chain fatty acids that are essential for many bodily functions.
The make-up of the intestinal flora can be influenced by a variety of factors. These include how we were delivered at birth, whether we were breastfed, how many germs we were exposed to during childhood, whether we were administered antibiotics, what infections we suffered, and our diet. The proportion of useful intestinal bacteria has dropped significantly for many people in the west. Indeed, the Western lifestyle is a culprit in the development of countless diseases. Probiotics are used to restore balance to the intestinal flora by introducing selected, useful bacteria to the digestive process.
Alongside bacterial cultures that can reproduce, probiotics usually also contain a growth substrate that promotes only the growth of the particular bacteria they contain, and as selectively as possible. In theory, this does apply to lactose, but the nature of the digestive process means lactose cannot reach the large intestine, where the bacteria is intended to settle, in significant enough quantities, because it has already been largely absorbed by the small intestine. Therefore lactose is not a suitable substrate for probiotics. Instead, we must rely on fibers that cannot be absorbed in the small intestine, such as inulin or oligofructose.
There are several reasons why someone may not be able to tolerate probiotics, and often that reason is the growth substrate contained in the probiotic supplement. Inulin and oligofructose are a perfect breeding ground for useful intestinal bacteria (e.g. lactobacilli and bifidobacteria), but bacterial fermentation causes considerable gas emissions, which can lead to unpleasant digestive problems. However, this is compensated for by the production of short-chain fatty acids, which are an important nutrient for the intestinal mucosa.
Another cause of intolerance can be a significant shift in the balance of the intestinal flora (dysbiosis). If probiotic bacteria are introduced externally into the body, they attempt to alter the intestinal conditions in their favor, and do so very radically. They produce lactic acid to acidify the environment, as well as other antibiotic substances to drive away other germs. These germs react by defending themselves against the attacks, and this microbial conflict can lead to discomfort in the intestine.
One aspect of probiotic intolerance that is often overlooked is small intestinal bacterial overgrowth (SIBO). Normally the small intestine is only sparsely populated with bacteria, but when we fall ill, this can lead to excessive bacterial growth in the small intestine. If you take probiotics with SIBO, the bacteria and their growth substrate may accelerate improper colonization of the small intestine. This development is often accompanied by severe digestive problems. For this reason, our recommendation is to take probiotics in consultation with a doctor.
Probiotics can cause severe digestive discomfort when you first take them. To alleviate this, it can be helpful to start off slowly. For example, consider opening the capsule and only using a fraction of the contents, increasing the dosage slowly and gradually.
To prevent flatulence, you can also empty a capsule into a glass of water and wait approximately 30 minutes before drinking it. During this time, the bacteria can largely break down the substrate while they multiply. However, this step will undoubtedly reduce the probiotic’s effectiveness, since without the capsule, fewer bacteria will survive the gastrointestinal passage.
With probiotics, we usually have the choice between individual bacterial strains and a mixture of typically 8–10 different strains, and it may not always be obvious as to which one is appropriate. Clinical studies have clearly proven the effectiveness of selected individual strains with especially promising properties, but when dealing with many bacterial strains, it is more difficult – sometimes even impossible – to attribute an effect to a certain strain. The data on this is therefore significantly weaker, but that does not necessarily mean that probiotic solutions with several strains are less suitable.
In short, then, there is no perfect probiotic remedy. There are many interesting probiotic bacterial species, though many properties are strain-specific, hence it makes sense to rely on remedies that contain well-studied strains with specified properties. Incidentally, high-quality probiotics will always state these properties clearly (see screenshot).
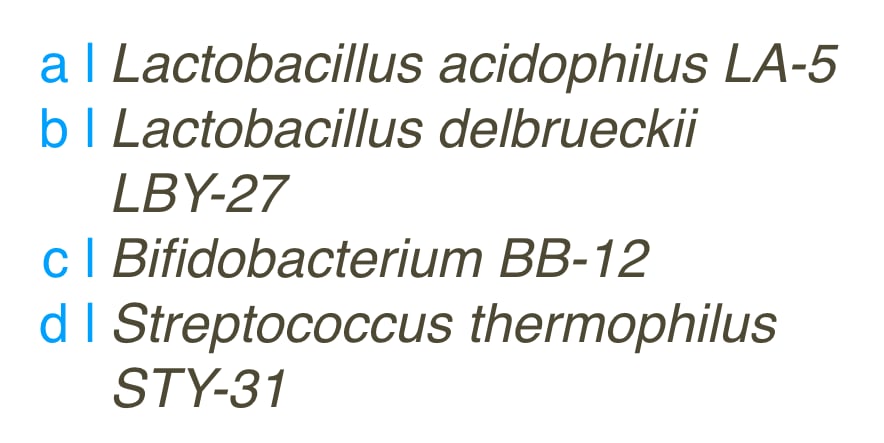 ▲Figure 1: Probiotic strains listed in detail indicate a high-quality probiotic. Many probiotics only list the bacterial cultures they contain with no specific details, e.g. L. casei.
▲Figure 1: Probiotic strains listed in detail indicate a high-quality probiotic. Many probiotics only list the bacterial cultures they contain with no specific details, e.g. L. casei.
Although numerous studies have shown lactic acid bacteria to have promising results, the question remains as to whether that positive effect is sustainable. It can be observed that the effect wears off a few days after you stop taking probiotics, and that most of the lactobacilli or bifidobacteria used as probiotics today do not form numerically significant populations in the intestine.
That doesn't mean that probiotics can't significantly improve your health, and even sustained colonization of the intestines is apparently not necessary for this. Nevertheless, we shouldn’t forget that the effect is only temporary in most cases, and the supply of probiotic bacteria must constantly be replenished. There is a long-term cost implication here that should be borne in mind.
There is likely to be significant progress and discovery in this field in the future, once probiotic bacteria that provide sustainable intestinal colonization have been identified. Another solution to intolerance could also be to take prebiotics that promote the growth of bacteria already present in the gut.
After having been niche foods for a long time, fermented foods such as unpasteurized sauerkraut, kimchi or kombucha are enjoying increasing popularity. They contain a variety of bacteria that are found naturally in the body and are valuable for our intestinal flora, as opposed to a small number of bacterial cultures with clearly labelled properties that are found in many supermarket products. With fermented foods. Fermented foods can contribute significantly to a balanced intestinal flora – we consume not only their bacteria but also their metabolic products – and regular consumption has been proven to reduce many inflammatory markers in the body.
Unfortunately for histamine intolerance sufferers, it is those metabolic products that often make these foods intolerable. The wild mix of microorganisms also contains many producers of histamine and other biogenic amines. In that regard, therefore, probiotics are usually a better option than fermented foods.
 Our price-winning "Food Intolerances" app helps you manage your diet. Available for iOS and Android. Check it out:
Our price-winning "Food Intolerances" app helps you manage your diet. Available for iOS and Android. Check it out:
Share article
Back to blog
Sources:
Image:
Photo by The Matter of Food on Unsplash

Why do we need probiotics?
Our intestinal tract contains around 39 trillion microorganisms that help us break down indigestible food components – fiber, for example – for the body to make use of them. Most of the intestinal flora is found in the large intestine. Over time, the metabolic processes of many lactic acid bacteria and bifidobacteria have become closely interlinked with our own, resulting in a symbiosis that benefits both the bacteria and the host. The bacteria get nutrients and a fertile place to multiply and in return form vitamins and short-chain fatty acids that are essential for many bodily functions.
The make-up of the intestinal flora can be influenced by a variety of factors. These include how we were delivered at birth, whether we were breastfed, how many germs we were exposed to during childhood, whether we were administered antibiotics, what infections we suffered, and our diet. The proportion of useful intestinal bacteria has dropped significantly for many people in the west. Indeed, the Western lifestyle is a culprit in the development of countless diseases. Probiotics are used to restore balance to the intestinal flora by introducing selected, useful bacteria to the digestive process.
Do probiotics contain lactose?
Alongside bacterial cultures that can reproduce, probiotics usually also contain a growth substrate that promotes only the growth of the particular bacteria they contain, and as selectively as possible. In theory, this does apply to lactose, but the nature of the digestive process means lactose cannot reach the large intestine, where the bacteria is intended to settle, in significant enough quantities, because it has already been largely absorbed by the small intestine. Therefore lactose is not a suitable substrate for probiotics. Instead, we must rely on fibers that cannot be absorbed in the small intestine, such as inulin or oligofructose.
Why can’t I tolerate any probiotics?
There are several reasons why someone may not be able to tolerate probiotics, and often that reason is the growth substrate contained in the probiotic supplement. Inulin and oligofructose are a perfect breeding ground for useful intestinal bacteria (e.g. lactobacilli and bifidobacteria), but bacterial fermentation causes considerable gas emissions, which can lead to unpleasant digestive problems. However, this is compensated for by the production of short-chain fatty acids, which are an important nutrient for the intestinal mucosa.
Another cause of intolerance can be a significant shift in the balance of the intestinal flora (dysbiosis). If probiotic bacteria are introduced externally into the body, they attempt to alter the intestinal conditions in their favor, and do so very radically. They produce lactic acid to acidify the environment, as well as other antibiotic substances to drive away other germs. These germs react by defending themselves against the attacks, and this microbial conflict can lead to discomfort in the intestine.
When should you not take probiotics?
One aspect of probiotic intolerance that is often overlooked is small intestinal bacterial overgrowth (SIBO). Normally the small intestine is only sparsely populated with bacteria, but when we fall ill, this can lead to excessive bacterial growth in the small intestine. If you take probiotics with SIBO, the bacteria and their growth substrate may accelerate improper colonization of the small intestine. This development is often accompanied by severe digestive problems. For this reason, our recommendation is to take probiotics in consultation with a doctor.
How can I improve my tolerance to probiotics?
Probiotics can cause severe digestive discomfort when you first take them. To alleviate this, it can be helpful to start off slowly. For example, consider opening the capsule and only using a fraction of the contents, increasing the dosage slowly and gradually.
To prevent flatulence, you can also empty a capsule into a glass of water and wait approximately 30 minutes before drinking it. During this time, the bacteria can largely break down the substrate while they multiply. However, this step will undoubtedly reduce the probiotic’s effectiveness, since without the capsule, fewer bacteria will survive the gastrointestinal passage.
How do I find the perfect dose?
With probiotics, we usually have the choice between individual bacterial strains and a mixture of typically 8–10 different strains, and it may not always be obvious as to which one is appropriate. Clinical studies have clearly proven the effectiveness of selected individual strains with especially promising properties, but when dealing with many bacterial strains, it is more difficult – sometimes even impossible – to attribute an effect to a certain strain. The data on this is therefore significantly weaker, but that does not necessarily mean that probiotic solutions with several strains are less suitable.
In short, then, there is no perfect probiotic remedy. There are many interesting probiotic bacterial species, though many properties are strain-specific, hence it makes sense to rely on remedies that contain well-studied strains with specified properties. Incidentally, high-quality probiotics will always state these properties clearly (see screenshot).
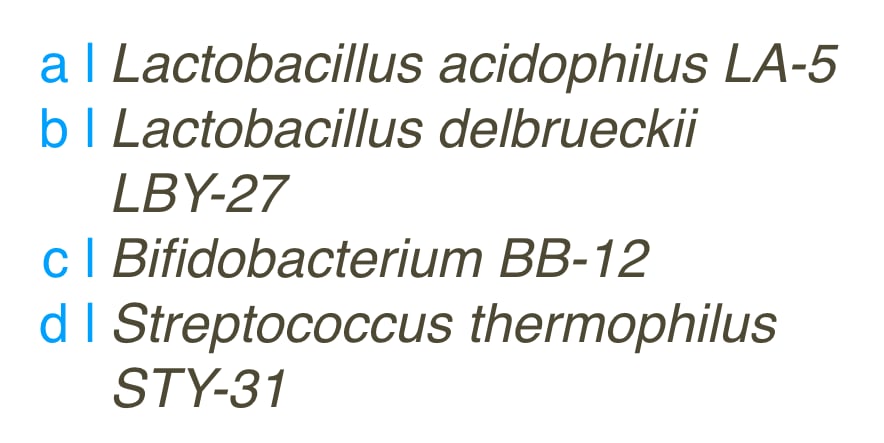
Caution: Unfortunately, the market for nutritional supplements is poorly regulated and it’s very easy to find low-quality probiotics. Information on the number or composition of a probiotic on the item label is often incorrect, or there may even be contamination with unwanted germs. It is therefore highly recommended to buy from trustworthy manufacturers who perform their own quality controls.
Are the effects of probiotics sustainable?
Although numerous studies have shown lactic acid bacteria to have promising results, the question remains as to whether that positive effect is sustainable. It can be observed that the effect wears off a few days after you stop taking probiotics, and that most of the lactobacilli or bifidobacteria used as probiotics today do not form numerically significant populations in the intestine.
That doesn't mean that probiotics can't significantly improve your health, and even sustained colonization of the intestines is apparently not necessary for this. Nevertheless, we shouldn’t forget that the effect is only temporary in most cases, and the supply of probiotic bacteria must constantly be replenished. There is a long-term cost implication here that should be borne in mind.
There is likely to be significant progress and discovery in this field in the future, once probiotic bacteria that provide sustainable intestinal colonization have been identified. Another solution to intolerance could also be to take prebiotics that promote the growth of bacteria already present in the gut.
Which is better for histamine intolerance: probiotics or fermented foods?
After having been niche foods for a long time, fermented foods such as unpasteurized sauerkraut, kimchi or kombucha are enjoying increasing popularity. They contain a variety of bacteria that are found naturally in the body and are valuable for our intestinal flora, as opposed to a small number of bacterial cultures with clearly labelled properties that are found in many supermarket products. With fermented foods. Fermented foods can contribute significantly to a balanced intestinal flora – we consume not only their bacteria but also their metabolic products – and regular consumption has been proven to reduce many inflammatory markers in the body.
Unfortunately for histamine intolerance sufferers, it is those metabolic products that often make these foods intolerable. The wild mix of microorganisms also contains many producers of histamine and other biogenic amines. In that regard, therefore, probiotics are usually a better option than fermented foods.
 Our price-winning "Food Intolerances" app helps you manage your diet. Available for iOS and Android. Check it out:
Our price-winning "Food Intolerances" app helps you manage your diet. Available for iOS and Android. Check it out:Share article
Back to blog
Sources:
- https://de.wikipedia.org/wiki/Mikrobiom (abgerufen 08/2022)
- M. Hrubisko et al., Histamine Intolerance—The More We Know the Less We Know. A Review, Nutrients 13:2228 (2021), 1–21
- https://gold.jgi.doe.gov/organisms?page=1&asc=Organism.Organism+Name&Study.Relevance.ID_options=or&Organism.Organism+Name=Lactobacillus+casei&count=500
- W. Barcik et al., Immune regulation by histamine and histamine-secreting bacteria, Current Opinion in Immunology 48 (2017), 108–113
- M. Schink et al., Microbial patterns in patients with histamine intolerance, Journal of Physiology and Pharmacology 69:4 (2018), 579–593
- H. Wastyk et al., Gut-microbiota-targeted diets modulate human immune status, Cell 184 (2021), 4137–4153
- T. Chen et al., Microbiological quality and characteristics of probiotic products in China, Journal of the Science of Food and Agriculture 94:1 (2013), 131–138
- D. Mazzantini et al., Spotlight on the Compositional Quality of Probiotic Formulations Marketed Worldwide, Frontiers in Microbiology 12 (2021), 1–16
- S. Fijan, Microorganisms with Claimed Probiotic Properties: An Overview of Recent Literature, Int. J. Environ. Res. Public Health 11 (2014), 4745–4767
- J. Walter, Ecological role of Lactobacilli in the gastrointestinal tract: Implications for fundamental and biomedical research. Appl. Environ. Microbiol. 74 (2008), 4985–4996
Image:
Photo by The Matter of Food on Unsplash
![[Blog]](../../rw_common/images/baliza_logo_retina.png)

